Osteoarthritis is a chronic joint disease, accompanied by pathological changes in hyalin cartilage, then in adjacent tissues, a joint capsule and a synovial shell.
The defeat is dystrophic and degenerative in nature, which leads to a change in the structure of joint tissues, the loss of their functionality.In accordance with the data of the same statistics, osteoarthritis is subject to 12% of the total population of the planet.From 62% to 65% of all the episodes of the disease falls to people over 60 years of age.
30 to 35% of cases of joint lesions to this pathology are in patients aged 40 to 60.And around 3% are young people aged 20 to 40.
What is this?
In simple terms, osteoarthritis is a chronic disease in which dystrophic degenerative progressive changes develop in the joint due to a violation of metabolic processes.It is the most common joint pathology, is diagnosed in 6 to 7% of the population.With age, the incidence increases considerably.
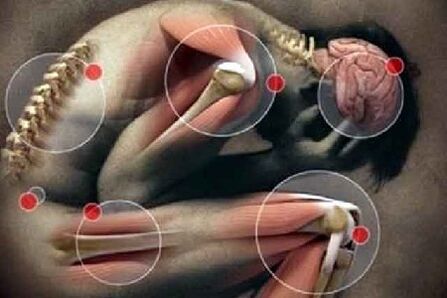
Most often, with osteoarthritis, the small joints of the brush are involved in the pathological process (in women 10 times more often than in men), the thumb of the foot, the intervertebral joints of the chest and cervical spine, as well as the knee and hip joints.The osteoarthritis of the knee and hip joints occupies a leading place in terms of severity of clinical manifestations and a negative effect on quality of life.
Arthrosis is characterized by global damage to joint and auxiliary devices:
- Chondrite - Inflammatory changes in the cartilage of the joint;
- Osteitis - damage to the pathological process of the subject's bone structures;
- Synovitis - Inflammation of the inner shell of the joint capsule;
- BURIT - Defeat of the Périoséman bags;
- Reactive inflammation of soft tissues (muscles, subcutaneous fibers, ligament devices) located in the projection of the involved joint (periarticular inflammation).
The disease is detected in 2% of people under the age of 45, 30% from 45 to 64 years and 65 to 85% from 65 and over.The greatest clinical importance, due to their negative impact on the standard of living and the capacity of patients, is osteoarthritis of large and medium joints of the limbs.
Types of osteoarthritis
Depending on the cause of the pathological process, primary, secondary and idiopathic osteoarthritis is distinguished within the joint.
The primary develops as an independent, secondary disease, following an injury or an infection, and the cause of the idiopathic form is not known.In addition to the classification of the disease, depending on the cause of the pathological process, osteoarthritis is distinguished instead of location of destructive changes:
- Gonarthrosis is the most common type of pathology, characterized by damage to the knee joints.Most often, gonarthrosis is detected in people with an excess weight, with chronic metabolic diseases in the body, low immunity.Knee osteoarthritis is progressing for a long time and gradually leads to a complete loss of the motor function.
- The osteoarthritis of the shoulder joint is the main cause of degenerative processes in this area are congenital anomalies in the development of the shoulder joint or excessive charges on this area, for example, when wearing heavy treasures on the shoulders.
- The ankle osteoarthritis - The main causes of the development of degenerative processes in the ankle joint are injuries, dislocations, stretching, fractures.In some cases, the development of the pathological process can cause an autoimmune disease - rheumatoid arthritis.Ankle osteoarthritis is subject to dancers, women wearing high heels, athletes.
- Non -Joarthrosis or osteoarthritis in the cervical region - causes are neck injuries, the progression of osteochondrosis, obesity, inactive lifestyle.At risk, people working on the computer are in offices.In addition to the intense pain in the neck, patients pronounced stunning, inhibition of consciousness, memory and fatigue disorders.These symptoms are due to the compression of the vertebral artery through which nutrients and oxygen penetrate the brain.
- Coksartrose or osteoarthritis of the hip joint - The main cause of occurrence is age -related changes in the tissues of the joint.At risk, people over 45.
- Fingers' osteoarthrosis - is developing for the same reason as spondylrosis.
- Polyrthrosis - characterized by damage to several joints with progressive degenerative processes, while ligaments, muscles and tissue joints are involved in the pathological process.
- Spondylarthrosis - destructive destruction is subject to the tissues of the spine, namely its lumbar service.To the risk group of a woman during the occurrence of menopause, since spondylrosis progresses in the context of a deficiency of female sex hormones.
The causes of osteoarthritis
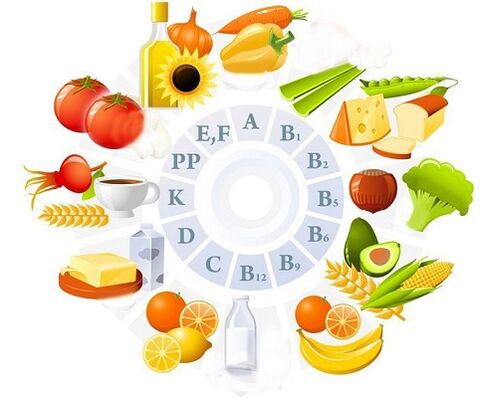
The formation of osteoarthritis is facilitated by two causes - the load and the absence of a complete nutrition which provides vitamins, minerals for the restoration of fabrics.The joints of each person carry a charge.Athletes and dancers, with physical work, the load on their feet is greater, which means that the bone joints wear out more quickly and require high quality nutrition.With a calm lifestyle, the support device wears slower, but also requires periodic renewal of fabrics.
Consequently, the main condition for the destruction and deformation of the joints is lower nutrition, the fact of not having disassembled the useful components, which often occur in the event of metabolic disorders.
We list the factors that contribute to the wear of joint compounds and metabolic disorders:
- Muscle weakness and incorrect load of the joints.The weakening of one or more muscles increases the load on the joint and the distributes unevenly inside the bone compound.An incorrect muscular load is also formed for flat feet, scoliosis, therefore, with these "harmless" diseases with age, cartilage tissues wear out, osteoarthritis appears.
The probability of osteoarthritis increases with a very physical effort.
If the daily loads exceed the capacities of bone tissue, microtraumas are formed.Thickness occurs in places of injury, which over time develop and deform the joint;
- Metabolic disorders (gastrointestinal disease - stagnation of bile, dysbiosis, gastritis, cholecystitis, pancreatitis, metabolic disease - diabetes);
- Psychosomatic causes - osteo psychosomatics confirms that the cause of the disease becomes a negative emotional state.Stress forms muscle spasms, constant stress disrupts the nutrition of all tissues (internal organs, bone, joints);
- Heredity (the type of metabolism is inherited and its possible violations, a tendency to muscle weakness or the incorrect formation of the bone apparatus, to poor digestion - which is the basis of the development of osteoarthritis in old age).
Osteoarthritis is a disease of the worn joints that have lost a significant supply of mineral substances and the ability to counter loads and destruction.Therefore, with age, predisposition to the disease increases.After 70 years, osteoarthritis is diagnosed with each second pensioner.Since the maximum load falls on the feet (a person moves - walks, gets up, short, jumps), then it is here that the first signs of osteoarthritis are formed.
The mechanism of progression of the disease
When one of the causes that cause the disease of joint with osteoarthritis appears, pathological processes are starting to develop there.The mechanism of their progression is not entirely studied, but the main stages of official medicine are known.
At the initial stage, the structure of the cartilage fabric and abnormal changes in the synovial fluid occur.All this takes place due to violations of the metabolic processes in which joint tissues do not receive the necessary components in sufficient quantities or are deprived of some of them.
Then, the elasticity of collagen fibers and the flexibility of cartilage are lost, because, with a lack of nutrients, hyaluronic acid does not have time to produce the softness and flexibility of the structural composition of collagen fiber.The cartilage dry gradually becomes brittle and cracks.The liquid in the synovial capsule is gradually exhausted and then disappears completely.
On the fabric of the cartilage, roughness, solid bone neoplasms form.At the same time, the deformation of other joint tissues develops, their pathological degeneration, their dystrophy and the loss of physiological activity.For the patient, these changes mean the appearance of pain, lameness and the immobility of the joint.
Osteoarthritis
Osteoarthritis is not characterized by an acute clinical picture, changes in the joints are progressive, slowly growing, which manifests itself by a gradual increase in symptoms:
- pain;
- Crunch periodically on the affected joint;
- the joint deformation that appears and improves as the disease progresses;
- rigidity;
- Restriction of mobility (reducing the volume of active and passive movements in the affected joint)
Pain in osteoarthritis is stupid transient, appears during the trip, in the context of an intensive load, at the end of the day (it can be so intense that it does not allow the patient to fall asleep).The constant and non-grustal nature of the pain for osteoarthritis is not characteristic and indicates the presence of active inflammation (subchondral bone, synovial membrane, ligant or periarticular muscles).
Most patients noted the presence of SO start -up pains that occur in the morning after waking up or after a long period of inaction and passage during motor activity.Many patients define this condition as the need to "develop a joint" or "disperse".
Arthrosis is characterized by morning stiffness, which has a clear location and is in the short term (no more than 30 minutes), sometimes it is perceived by patients as a "jelly feeling" in the joints.Perhaps a feeling of jamming, stiffness.

With the development of a reactive synovitis, the main symptoms of osteoarthritis are joined:
- Pain and local increase in the temperature determined by the palpation of the affected joint;
- constant nature of pain;
- increase in the joint in volume, swelling of soft tissues;
- Gradual reduction in the volume of movements.
Stages and degree of osteoarthritis
During illness, medicine distinguishes three stages that have differences in signs of the disease, the intensity of damage and location.At the same time, the differences in the three stages are linked to the types of tissues that suffer from pathological changes.
- The first degree of development of joint osteoarthritis is the initial phase of the disease.It is characterized by a slight lesion of cartilage tissue and the loss of physiological functions in collagen fibers.At the same time, at the first stage, the minor morphological disorders of the bone tissue and the structural changes of the synovial fluid are noted.The cartilage of the joint is covered with cracks, the patient suffers from a slight pain in the location of the pathology.
- The second degree is the development of osteoarthritis with an increase in dynamics.This step is characterized by the appearance of stable pain, chroma.Notable morphological and dystrophic cartridges of cartilage are noted, during the diagnosis, bone growths are revealed.Osteophytes are formed - bone growths which are visible during a visual examination of the destruction site.At the same time, the processes of degenerative changes in the synovial capsule occur, which leads to its structural exhaustion.The disease of this phase can often worsen and be regular.The pain becomes gradually constant.
- The third degree is an active progression.At this stage, the synovial fluid is almost completely absent due to its degeneration and sudden bone tissue on each other.Joint mobility is almost completely absent, the pain becomes more tangible.The cartilage fabric is also absent due to degenerative and atrophic changes.The third degree of arthritis of the joints is considered to be impractical.
In addition to these three degrees of pathology development, there is a final stage - irrevocable destruction of all joint tissues.In this phase, it is impossible not only to lead productive therapy, but even to eliminate pain syndrome.
The inflammatory process generally begins with a second degree of damage, in rare cases, in the absence of medical intervention - at the first stage.Thereafter, it becomes more difficult to stop it, which can lead to secondary pathologies, the development of pathogenic microflora in place of the location of the disease.
To exclude serious consequences, treatment should start from the first degree and the use of intensive care methods.At the last stage associated with the complete destruction of the cartilage fabric, a single methodology for driving the patient of pain and the immobility of the joint is authorized - the endoprothetics with a complete or partial replacement of the components of the joint.
Consequences
The consequences of premature treatment and launched arthritis of the joints are heavy with complications such as:
- disability;
- deformation without possibility of recovery;
- the appearance of vertebrates;
- an inactivity or the immobility of the joint;
- Reduce quality and standard of living.
The chronic course, in addition to these complications, is accompanied by intense and frequent pain, the complete destruction of the structural components of the articulation, the discomfort, the inability to do physical work and practical sports.
Diagnosis
The diagnosis of osteoarthritis is based on the evaluation of anamnestic data, the manifestations characteristic of the disease, the results of the instrumental research methods.Indicative changes in general and biochemical blood tests for osteoarthritis are not characteristic, they only appear with the development of an active inflammatory process.
The main instrumental method for diagnosing osteoarthritis is radiography, in clear diagnostic cases, computation or magnetic refusal is recommended.
The osteoarthritis of the knee and hip joints occupies a leading place in terms of severity of clinical manifestations and a negative effect on quality of life.
Additional diagnostic methods:
- Atraumatic arthroscopy;
- ultrasound (evaluation of the thickness of the articular cartilage, synovial shell, condition of the joint bags, presence of liquid);
- Scintigraphy (assessment of the state of the bone tissue of the bones which form the joint).
How to treat osteoarthritis?
It is preferable to treat arthritis of joints at an early stage, the treatment itself should be pathogenetic and complex.Its essence is to eliminate the causes that contribute to the development of this disease, it is also necessary to eliminate inflammatory changes and to restore the functions that have been lost earlier.
The treatment of osteoarthritis is based on several basic principles:
- Saturation of the joint with oxygen, or intra-articular oxygen therapy if called.
- Therapy with drugs.
- Intra-fosal blockade, as well as the decompression of the metaepay.
- Rational approach to nutrition.
- Damaged joints should be eliminated from excessive load.If possible, during treatment, it should generally be reduced to a minimum.
- According to the established orthopedic diet.
- Classes of physiotherapy exercises.
- The passage of physiotherapy, which includes a magnet and electrotherapy, a shock wave, as well as laser therapy.
- Treatment of sanatorium.To do this, it is necessary once a year, on the recommendation of a doctor, undergoes a course treatment in specialized stations.
Preparations for the treatment of osteoarthritis
The drug treatment is carried out in the exacerbation phase of osteoarthritis, selected by a specialist.Self-medication is unacceptable due to the possible side effects (for example, the negative effects of non-steroidal anti-inflammatory drugs on the gastric mucosa).
Therapy includes the objective of these drugs:
- Anti-inflammatory drugs.The start of osteoarthritis therapy is complete, you can slow down the course of the disease and largely improve quality of life.It is worth lingering in more detail at certain treatment points.In particular, therapy with drugs includes at the initial stage - it is the elimination of pain, as well as the elimination of inflammatory processes occurring in the joints.For this, all doctors use non-steroidal anti-inflammatory drugs.Experienced doctors do not recommend their oral use, as these drugs largely irritate stomach walls.Therefore, depending on the medication chosen, intravenous or intramuscular administration is used.Sometimes, as auxiliary means, NSAIDs are used in the form of ointments, but their absorption is extremely low, so it is not possible to obtain a significant effect.
- Hormonal corticosteroids.When osteoarthritis is at the stage of exacerbation, hormonal corticosteroids are recommended.They are inserted in the joint.Externally, you can use a special patch, ointment or dye, which are made on the basic pepper base.
- Chondroprotectors aimed at restoring cartilage and improving the high quality composition of synovial fluid will not be superfluous.The course lasts a fairly long period until the moment until the improvement occurs.However, if the expected effect does not appear on one U-turn, the drugs must be canceled.As intra-fast, as well as chondroprotectors, it is advisable to use drugs made on the basis of hyaluronic acid.They contribute to the formation of a cell membrane responsible for the formation of a cartilage of the joint.
Physiotherapeutic treatment
To stop pain, reduce inflammation, improve microcirculation and eliminate muscle cramps from the patient with osteoarthritis, is directed to physiotherapy:
- In the exacerbation phase.Prescribe laser therapy, magnetotherapy and ultraviolet irradiation,
- In the remission phase.Electrophoresis and phonophoresis are displayed.
In addition, thermal procedures are used, sulfide, radon and sea baths. To strengthen muscles, electrical stimulation is carried out.A soft massage can also be used in the remission phase.
Surgical treatment
With the ineffectiveness of these exposure methods, in the presence of complications, resort to surgical treatment of osteoarthritis:
- Decompression of the metaepinating and prolonged intraossers (decrease in intraosseuse pressure in the affected area);
- Corrective osteotomy;
- Actoprosthetics of the joints.
In the first stages of the disease, a mechanical, laser or cold debate (smoothing of the damaged cartilage surface, the elimination of non -viable areas) are used.This method effectively stops pain syndrome, but has a temporary effect 2-3 years.
Folk remedies
Most people of our time do not want to take pills or do injections.Therefore, they wonder - how to cure osteoarthritis using folk remedies?For the most part, these funds aim to increase the tone of the body, improve blood circulation, relieve pain and increase immunity.
For the treatment of this disease, such recipes for traditional medicine are used:
- The egg solution is prepared from fresh egg yolk, which is mixed with turpentine and apple cider vinegar in a ratio of 1: 1: 1. The liquid must be carefully mixed and grate it with the assigned joint for the whole night.Then you have to wrap everything with a wool scarf.It is recommended to make friction for 1 month 2-3 times a week.
- The pharmacy is bought by the Eleasil root.As a rule, it faces 50 g packages.For the preparation of the dye, it will take a half-packet of vegetable roots and 150 ml of high quality vodka.The ingredients are mixed, placed in a dark bottle and insisted for 12 days.The friction is done before bedtime, and if possible in the morning.
- The use of boiled oats also gives good results.Take three or four spoons of oat flour, pour boiling water and cook over low heat for five to seven minutes.The amount of water used must ensure the reception of the thick porridge, which must be cooled and used as a compress at night.Use only boiled flakes recently.The porridge of yesterday for the compress is not suitable.
- The birch leaves, the nettles and the inflorescence of the calendula are caught.As a result, you should get two tablespoons.We fold the resulting chopped collection in a thermos, pour a liter of boiling water and leave it during the night.From morning in the morning, it is necessary to take half a glass of decoction four to five times a day.The course of taking this recipe is two to three months.

Taintings of bay, horseradish, garlic and rye grains are also considered effective.Treatment of osteoarthritis with folk remedies will be the most effective if you combine it with treatment with drugs.
Ostens up for osteoarthritis
The basic principles of nutrition for osteoarthritis are reduced to the following points:
- Do not eat heavy food for the night so as not to cause an osteoarthritis attack.
- Eat fractionally.
- Constantly monitor the weight, to avoid increasing body weight,
 And this means an additional load on the painful joints.
And this means an additional load on the painful joints. - When there is no exacerbation of the disease, hiking after eating.
- The menu must be balanced, compiled with the attending physician.
There is absolutely no complaint regarding fish dishes - they can be used a lot, of course, in reasonable quantities.
- Do not forget the regular consumption of vitamins with food.For patients with osteoarthritis, B vitamins are particularly relevant
- An important role in the treatment of osteoarthritis is attributed to cold man.Such food will be a real warehouse of elements for the painful joints.The most important component of the cold is a collagen of natural origin.
- Vitamin B will help the production of hemoglobin.It can be "obtained" by eating bananas, nuts, cabbage and potatoes.It is worth getting carried away by greenery and legumes.They will become a source of folic acid.The liver, mushrooms, dairy products and eggs will be useful.They are rich in riboflavin.
By observing the therapeutic scheme prescribed by the doctor, it may be obtained that the disease withdraws and the damaged tissues are starting to recover.
Prevention
The prevention of osteoarthritis begins with good nutrition.It is necessary to try to reduce salt consumption, as well as foods that can disrupt metabolism.These include legumes, fatty meat, alcohol.The diet includes cabbage, green vegetables and fish.
For the prevention of osteoarthritis, it is necessary to attend physical education lessons, to do hot UPS.If possible, it is better to spend several kilometers on foot.It is also important to monitor your weight and prevent weight gain, as this will give an additional load on the inflamed joints.It is not recommended to take pills to lose weight because they can disrupt metabolism in the body.
Forecast
Life forecasts are favorable.The favor of social forecasts and labor depends on the speed of diagnosis and the beginning of treatment, is reduced when tightening the resolution of the issue of surgical treatment of the disease if necessary.



















