Osteoarthritis(osteoarthritis) is a joint disease characterized by degenerative changes in the cartilage covering the bone, that is, its destruction.
%20and%20normal%20cartilage%20(right).jpg)
The overwhelming majority of affected joints are the knee, hip, shoulder, and first metatarsophalangeal. Damage to other joints is much less common and is often secondary. In recent years, the disability caused by osteoarthritis has doubled.
Like any disease, osteoarthritis also presents risk factors for its development, which are actively studied today, and the list goes on and on each year. The main ones are considered to be:
- age;
- heredity;
- Metabolic disorders;
- increased body weight;
- osteoporosis;
- inadequate and irregular nutrition;
- Endocrine disorders;
- menopause;
- frequent hypothermia;
- trauma;
- arthritis (inflammation of the joint);
- foci of chronic infection or inflammation (for example, chronic tonsillitis).
- Varicose veins.
If you notice similar symptoms, see your doctor. Don't self-medicate - it's dangerous for your health!
Symptoms of osteoarthritis
Common symptoms of osteoarthritis include:
- pain during exertion;
- limitation of movement in the joint;
- feeling of stiffness in the morning, sensation of "cracking";
- pain after a long rest (the so-called "starting").
Joint pain is rarely sharp, more often painful or dull, and usually stops when resting. Symptoms are often wavy and can come and go without trying to treat. They can be mild, moderate or severe. Complaints in osteoarthritis can remain approximately the same for many years, but over time they progress and the condition worsens. Minor and moderate symptoms can be controlled at the same level, but the severe course of the disease can lead to chronic pain, inability to perform daily household activities, which leads to disability, up to disability.
Pathogenesis of osteoarthritis
theThe main nutrient medium for the joint is the synovial liquid. It also acts as a lubricating agent between the joint surfaces. A huge and major role in the development of osteoarthritis is attributed to metabolic processes in the joint and its structures. At the initial stage, when biochemical disorders develop in the synovial fluid, its properties decrease, which triggers the mechanism of destruction. The first to touch is the synovial membrane of the joint, which plays an important role as a membrane and is a kind of filter for the most important nutrient in cartilage - hyaluronic acid, preventing it from leaving its place ofmain work - the joint cavity. The saturation of the properties of the joint fluid determines its circulation, which cannot be done without regular movement of the joint itself. Hence the well-known expression "movement is life". The constant circulation of synovial fluid in the joint cavity is the key to a full-fledged metabolism. With a lack of nutrients, the cartilage thins, the formation of new cells stops, the joint surface becomes uneven, rough, with areas of defects. The relationship between diseases of the veins of the lower extremities (for example, varicose veins)and the development of metabolic disorders in the joints, mainly the knee, is known. The bone structure under the cartilage responds to the process with a compensatory mechanism - it thickens, becomes coarser and widens the coverage area, leading to the formation of exostoses and osteophytes, the main reason for the limitations and deformities of thejoint. The synovial fluid is saturated with inflammatory cells and decaying elements, the joint capsule in response to this thickens, becomes rough and loses elasticity, the soft tissues literally become dry (dehydration occurs), hencecomplaints of morning stiffness, "starting pains". The pathological process in the last stages prompts the body to activate the last compensatory mechanism - immobilization. At rest and in the so-called physiological position, the pain is minimal, the ligament apparatus is straightened as much as possible. In this position, the joint tends to fix itself, and it succeeds in the rapid formation of coarser exostoses, which "fix" the joint, and the patient loses the ability to move it completely. The muscles of such a limb are hypotrophied, become weaker and smaller. Such changes are already considered irreversible.
Classification and stages of development of osteoarthritis
The disease is divided into 2 large groups: primary (or idiopathic) and secondary. The first group develops either as a result of some obscure reason, or as a result of age-related changes. The second is characterized by clear causes and develops as a result of their pathological process (for example, against the background of tuberculosis, osteochondritis dissecans, subchondral necrosis, etc. )
Whatever the reasons that have been a factor in the development of osteoarthritis, there are 4 stages in its development:
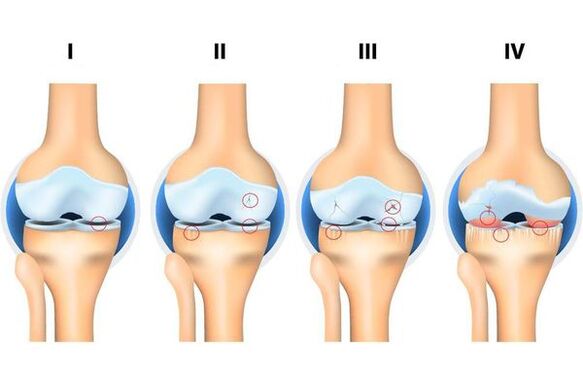
- Stage 1: The hard structures of the joint are not involved in the destruction process, there are initial changes in its soft structures and in the composition of the joint fluid (which is a nutrient medium and reduces the friction of the joint. joint), there is undernutrition of the joint.
- Stage 2: accompanied by the "start" of the mechanism of destruction of the solid structures of the joint, solid edge formations (exostoses, osteophytes) are formed. Moderate complaints of changes in range of motion.
- Stage 3: accompanied by narrowing of the articular lumen, pronounced destruction of the loaded surface with the formation of osteochondral defects, pronounced limitation of movements, constant feeling of "cracking" during movement, initial changes in the axis of the limb.
- Stage 4: severe, in which movements are clearly limited in the joint until its complete absence (ankylosis), a pronounced inflammatory process, its deformation, the formation of bone defects (due to the complete absence of cartilage cover).
Complications of osteoarthritis
Without treatment, any disease leads to complications, and osteoarthritis is no exception. If this is the primary form, the main complications are as follows:
- damage to the soft structures of the joint (degenerative tears of the menisci, tears of ligaments, etc. );
- chronic inflammatory process;
- ankylosis (complete lack of movement in the joint);
- deformation of the joint.
If it is a secondary form, the complications depend on the process that provoked the development of osteoarthritis. For example, it can lead to osteoporosis, a chronic disease characterized by a progressive disorder of bone metabolism. As a result, the bones become brittle, their nutrition is disturbed, as a result, osteoarthritis is complicated by the threat of intra-articular fractures. Therefore, it is so important to see a doctor in a timely manner. As the eminent surgeon wrote: "The future belongs to preventive medicine.
Diagnosis of osteoarthritis
The diagnosis of osteoarthritis often begins with a doctor (usually an orthopedic trauma specialist) from primary medical care (polyclinic), where a clinical examination is performed and the data from the examination (CT, MRI, X-rays, etc. )are interpreted to determine the degree and type of osteoarthritis. . . Diagnosis and diagnosis are generally straightforward. If the diagnosis is not clear or if the doctor suggests a secondary development of the disease, the patient is then referred, for clarification, to doctors of other specialties (for example, a rheumatologist). It is very difficult to determine the degree of osteoarthritis without examination results. The history of the disease, methods and attempts at treatment are also important for diagnosis and determining treatment tactics, as the doctor is often faced with the difficult task of differential diagnosis (for example, symptoms ofosteoarthritis and arthritis often coincide).
Osteoarthritis Treatment
Early stages of osteoarthritis, amenable to conservative treatment, provided an integrated approach. The treatment is long and pursues the main objective: either to stop the process of destruction at the stage when the treatment was started, or to slow down this process. The complex includes drug and non-drug therapy, which includes courses in exercise therapy (physiotherapy and gymnastics exercises), physiotherapy (usually phonophoresis and magnetotherapy), swimming, anti-inflammatory therapy (either byingestion, either topically in the form of gels or cream), chondroprotective therapy (taking medicines based on cartilage components) and intra-articular injections (these can be both homeopathic medicines and preparations of'hyaluronic acid). Chondroprotectors are still used by orthopedic traumatologists, they are prescribed by internal courses, but the results of recent scientific studies in Western countries refute the positive effect compared to the placebo effect. With severe symptoms and severe stages, conservative treatment becomes ineffective, putting surgical treatment in the first place. Given the indications, it can be both minimally invasive treatment - arthroscopy and endoprosthesis. With arthroscopy (endoscopy of the joint), it is disinfected under the control of video optics, exostoses (if possible) and damage to soft structures are removed, which is often observed at such stages. Recently, however, the benefits of this type of intervention for osteoarthritis have been increasingly questioned, as it does not have the desired effect in chronic pain, and in some cases it can cause severe pain. significant damage if improperly executed.
The stent is a technically difficult and difficult operation, the purpose of which is to create a completely new artificial joint. Requires clear indications and identification of risks in the presence of contraindications. Today, stents for the knee, hip and shoulder joints are used successfully. Additional outpatient monitoring by a doctor reduces the risks and conditions of rehabilitation, improves the quality and efficiency of the operation performed.
Forecast. Prophylaxis
The prediction depends on a timely visit to a traumatologist-orthopedist and the start of a treatment complex. In terms of the elimination of morphological changes in osteoarthritis, the prognosis is unfavorable, since it is impossible to completely restore the cartilage structure of the joint. In old age, the course of the disease is more severe than in young people. However, with timely access to a doctor and compliance with all recommendations, it is possible to eliminate all complaints and restore full motor function of the joint.
Preventive measures:
- Regular physical activity.It is a misconception that physical activity can "wear out" a joint. Increased - yes, but not regular and moderate. According to the latest data, any activity aimed at strengthening and maintaining muscle mass, improving coordination, supports the motor function of the joints and their blood supply. Any physical activity allows regular circulation of joint fluid, the main source of nutrition for the joint and its structures. It is known that people who use public transport every day and have foot traffic are less likely to develop osteoarthritis.
- Control of body weight and its adequate reduction.The increased mass increases the load on the joints of the lower extremities and spine. Thus, any rehabilitation and conservative treatment protocol for osteoarthritis includes a cure for LFT (physiotherapy and gymnastics exercises).
- Correction and elimination of congenital malformations.Flat feet play an important role, which over the years leads to a violation of the axis of the legs, which leads to a disproportionately increased load on some parts of the joints and spine, deforming them.
- Good nutrition.It allows you to create conditions for the complete enrichment of the joint with nutrients. Thus, the rejection of a large number of foods, frequent diets, irregular eating of foods low in substances (fast food, etc. ) can become a "trigger" for the development of osteoarthritis.
- Rapid elimination of concomitant diseases.Medical examinations, now forgotten, have made it possible to identify and eliminate diseases at an early stage. Concomitant diseases can be an important cause of the development and progression of osteoarthritis (for example, diseases of the endocrine system, gastrointestinal tract, chronic foci of infection or inflammation).



















